Abstract
Introduction: In the last few decades, there have been substantial improvements in outcomes of younger patients with Acute Lymphoblastic Leukemia (ALL). Unfortunately, similar results were not seen in the elderly population due to varied genetic makeup and lesser tolerance to aggressive pediatric-based treatment regimens. Lately, with developments, including novel therapeutics like Tyrosine Kinase Inhibitors (TKIs), Inotuzumab ozogamicin, Blinatumomab, CAR-T, significant improvements in survival have been noted. Our objective was to describe survival trends among elderly diagnosed with ALL in the last few years. We also described survival outcomes based on demographics and genetic features.
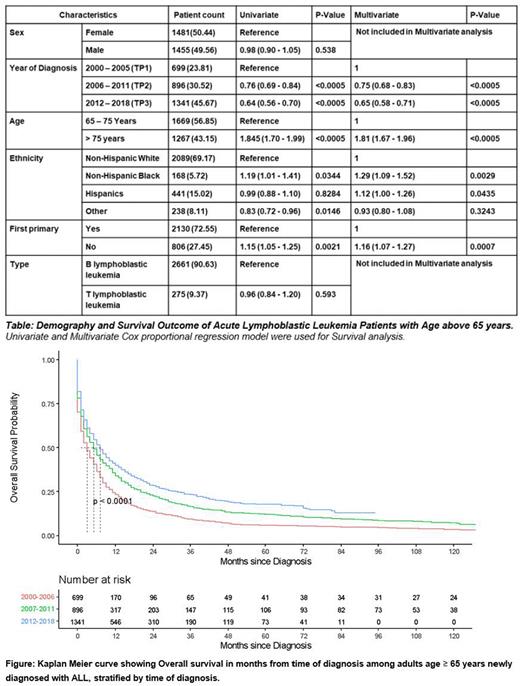
Methods: We identified patients with ALL aged ≥ 65 years from the Surveillance, Epidemiology and End Results (SEER) database for 2000-2018 period using WHO ICD-O-3 codes. Gender, age, race, histology, immunophenotype, genetic mutation (for patients diagnosed after 2010), prior malignancy status, year of diagnosis, survival months, and vital status, until the study cutoff (December 31, 2019) were collected. Years of diagnosis were divided into three study time periods (TP) [2000-2005 (TP1), 2006-2011(TP2), 2012-2018 (TP3)] to assess the effect of changing management strategies. Survival analysis was done using a Cox-proportional hazard regression model. Gender and immunophenotypic groups were not significant on univariate analysis and were not included in the multivariate analysis. Survival curves were plotted for each time periods by the Kaplan-Meier method and were compared using the log-rank test. Survival estimate were further compared for each time period for each subgroup of race (NHW and others), gender, immunophenotype and age group (>65-75 years,>75 years) with the posthoc comparison between each time period. The posthoc adjusted p value are calculated by bonferroni correction.
Results: A total of 26801 patients with ALL were identified. 10.02% (n=2986) were ≥65 years. After excluding cases with incomplete survival information (50 patients), 2936 patients were included for survival analysis. 50.44% (n=1481) were female. 69.17% (n=2089) patients were Non-Hispanic Whites. Clinically, it presented as secondary malignancy in 27.45% (n=806) patients. In terms of immunophenotypic subtype, 90.63% (n=2661) patients had B-Lymphoblastic leukemia, and 9.37% (n=275) had T- Lymphoblastic Leukemia [Table]. In terms of genetic mutations (data available only after year 2010), t(9;22) positive disease constituted 8.25% (n=139) of the total patients. In the survival analysis, superior outcomes were seen in patients with t(9;22) [HR 0.68 (95%CI 0.55-0.84)] with reference to B-Lymphoblastic Leukemia, NOS. Inferior outcomes were seen when ALL was diagnosed as a secondary malignancy [HR 1.16 (95% CI 1.07 - 1.27)] and for Non-Hispanic Black [HR 1.29 (95% CI(1.09-1.52)] with reference to Non-Hispanic White. Survival trends among the elderly population continued to improve over the study TPs 2000-2005 (Ref), 2006-2011 [HR 0.75 (95% CI 0.68-0.83)], 2012-2018 [HR 0.65 (95% CI 0.58-0.71)]. On subgroup analysis, Survival improved over the three time periods (TP1 to TP2, TP2 to TP3, TP1 to TP3) for Age group 65-75 years (p-values <0.005, 0.002 and <0.005), Non-Hispanic white (p-values <0.005, 0.006 and <0.005), B-cell immunophenotype (p-values <0.005, <0,005 and <0,005) and female patients (p-values <0.005, 0.005 and 0.0005). Improved survival from TP1 to TP2, and TP1 to TP3 were seen for Age group >75 years (p-value <0.009 and <0.0004), Other race (p-value 0.045 and <0.005), and Male (p-values <0.005 and 0.005) but there was no improvement seen over TP2 to TP3 for Age group >75 (p-value 1), Other race (p-value 0.096), and Male gender (p-value 0.35). For T cell immunophenotype, improved survival was only seen from TP1 to TP2 (p-value 0.018). Kaplan-meier curve were plotted for overall survival for the three time periods showing significant improvements as shown in the Figure (p-values <0.005, <0.005 and <0.005).
Conclusion: Overall prognosis for elderly patients diagnosed with ALL has improved in the last two decades. Notable improvements are seen in patients with t(9;22), owing to the use of TKIs. Study outlines racial disparity, as evident by poor outcome in Non-Hispanic Blacks. There are unmet needs of improvement in racial minorities, age >75 years and patients with T-cell immunophenotype.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal